Engage hard-to-reach members. Improve chronic disease outcomes.
Oben connects every touchpoint required to deliver value-based care in trusted community settings through a single platform, enabling: preventative screenings, clinical oversight, referral and navigation workflows, reimbursement and reporting.
Our team is ready to walk you through the Oben Health experience
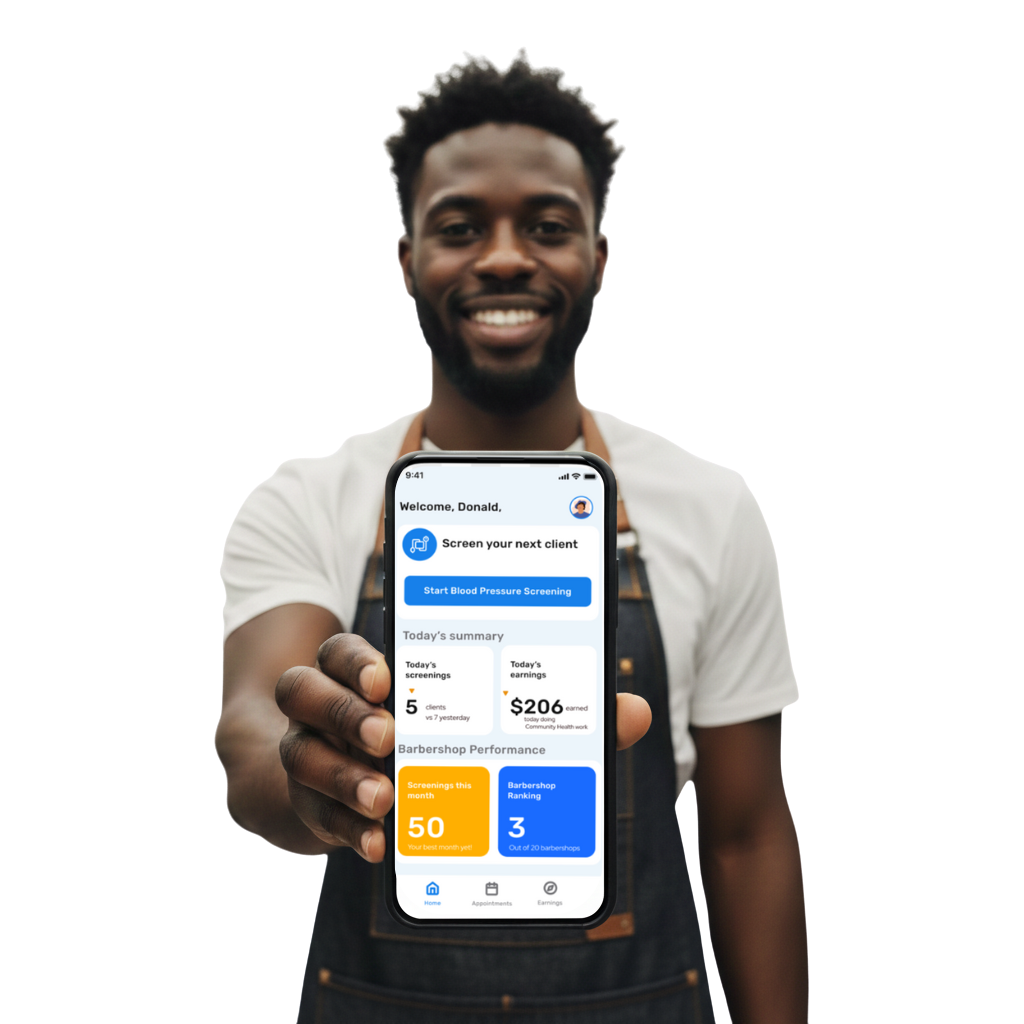
Seamlessly integrate care into routine workflows
We partner with barbers and stylists—training and credentialing them as certified Community Health Workers—so they can screen clients, capture vitals, and support care navigation in just minutes.
What the app enables:
Fast, guided screenings
Step-by-step clinical workflow
Patient education + support
Automated documentation + earnings tracking
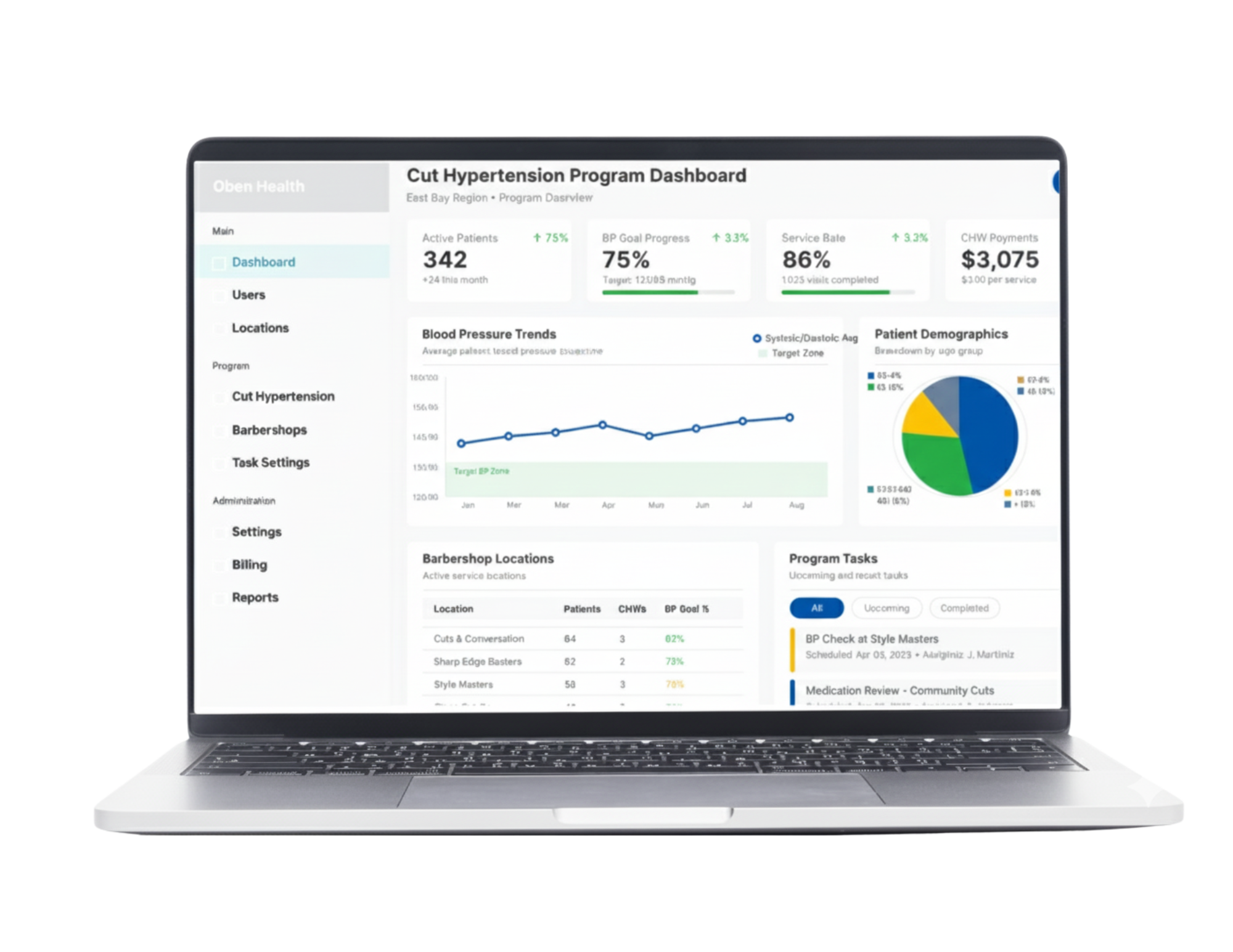
Triage Patient Care
Remote oversight + care planning at population scale
Gives clinicians the insight and tools needed to guide care remotely and intervene early — between appointments and outside the clinic.
What the platform enables:
Patient engagement back into primary care
Continuous patient monitoring with real time analytics
Risk stratification + prioritization
Faster escalation + follow-up
Integrated communication with community health workers
Engage Members And Close Care Gaps
Improve quality performance and reduce avoidable spend
Track engagement rates, screening outcomes, referrals, and financial performance from community-based care programs.
Traditional outreach misses high-risk members. Distributed care through trusted community spaces enables early intervention and prevents costly events later.
What the platform enables:
Real-time monitoring of community engagement
Automated documentation + claims tracking
Visibility into referral + follow-up completion
Insights tied to quality metrics + ROI